In Thailand, children’s risk of dying before age 5 varies more than four-fold
An unprecedented study mapping child deaths over almost two decades finds that the likelihood of a child reaching age 5 varies up to four-fold among districts in Thailand.
The research shows that in Thailand, 5,807 children died before their fifth birthdays in 2017, as compared to 18,509 in 2000. The highest district-level mortality rate was 19.6 in Sangkhla Buri. The lowest was 4.5 in Ban Kruat. Neonatal disorders were the biggest causes of deaths before age 5 in both 2000 and 2017, according to the Global Burden of Disease study, but the total number of deaths from these disorders more than halved during the study period.
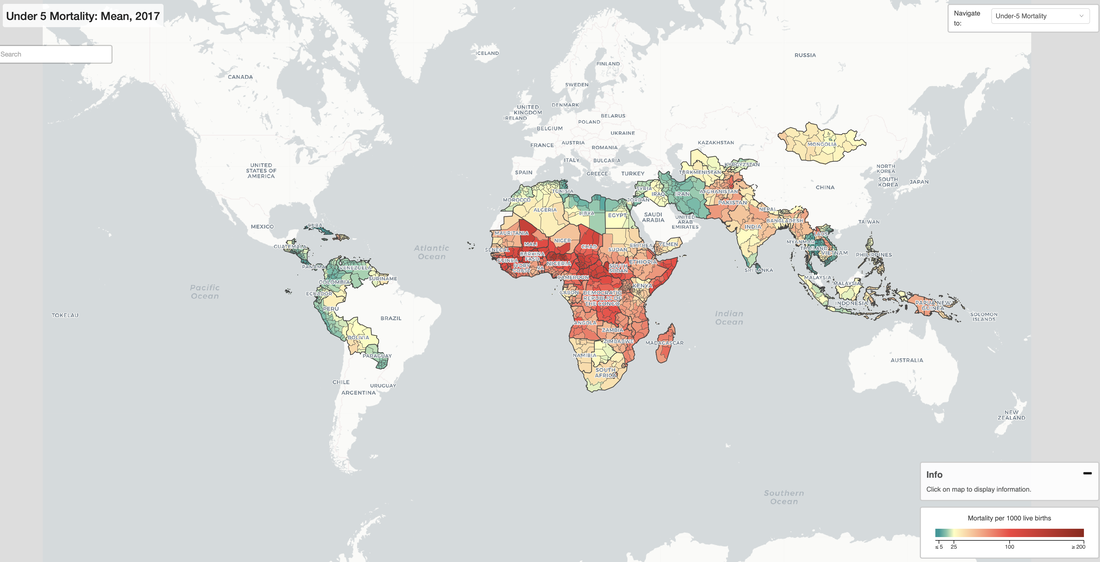
The study is the first of its kind, mapping child deaths in 99 low- and middle-income countries at the level of individual districts, municipalities, and provinces. Published today in the journal Nature, the findings include precision maps illuminating health disparities within countries and regions often obscured by national-level analyses. An interactive visualization accompanying the research compares child death rates from year to year.
The research shows that in Thailand, 5,807 children died before their fifth birthdays in 2017, as compared to 18,509 in 2000. The highest district-level mortality rate was 19.6 in Sangkhla Buri. The lowest was 4.5 in Ban Kruat. Neonatal disorders were the biggest causes of deaths before age 5 in both 2000 and 2017, according to the Global Burden of Disease study, but the total number of deaths from these disorders more than halved during the study period.
The study is the first of its kind, mapping child deaths in 99 low- and middle-income countries at the level of individual districts, municipalities, and provinces. Published today in the journal Nature, the findings include precision maps illuminating health disparities within countries and regions often obscured by national-level analyses. An interactive visualization accompanying the research compares child death rates from year to year.
The research, conducted by the Institute for Health Metrics and Evaluation (IHME) at the University of Washington’s School of Medicine, looks at countries where more than 90% of child deaths occurred in 2017. Across all countries studied, the likelihood of a child dying before age 5 varied more than 40-fold at the district level.
Researchers estimated that if every district in the low- and middle-income countries studied had met the Sustainable Development Goal (SDG) target of at least as low as 25 child deaths per 1,000 live births, 2.6 million fewer children would have died. If every district within a country rose to the level of the best-performing district in that country, the estimated number of deaths averted rises to 2.7 million.
The vast majority of the 17,554 districts among the 99 nations studied saw improvement in lowering child deaths, but levels of inequality between districts were more variable over the study period. Despite major gains in reducing child deaths over the past 20 years, the highest rates of death in 2017 were still largely concentrated where rates were highest in 2000.
“It is as reprehensible as it is tragic that, on average, nearly 15,000 children under age 5 die every day,” said Dr. Simon I. Hay, the senior author on the study and Director of the Local Burden of Disease (LBD) group at IHME. “Why are some areas doing so well, while others struggle? In order to make progress, we need to enable precise targeting of interventions, such as vaccines. Our findings provide a platform for nations’ health ministers, clinicians, and others to make focused improvements in health systems.”
The study, funded by the Bill & Melinda Gates Foundation, reveals areas of success where strategies could be replicated across and within countries, according to Dr. Hay.
For example, in Rwanda, the highest district-level rate of child deaths in 2017 was less than half that of the lowest district-level death rate in 2000 – gains partially attributed to investments in children’s health in the poorest communities, expansion of health insurance, and increasing numbers of community health workers. Nepal significantly decreased inequalities among its districts over the study period. And Peru made major strides in reducing child mortality and inequality after implementing sustained, cross-cutting antipoverty and health programs.
The study estimates both rates and absolute numbers of deaths by district, presenting a complete picture of global child mortality that illuminates important trends and patterns.
A growing proportion of child deaths are occurring in areas with low overall death rates. Neonatal mortality (death occurring in a child’s first 28 days) and infant mortality (death in the first year of life) are both increasing as a percentage of total child deaths. These trends highlight the need for tailored approaches.
Hay and his research team are working toward more detailed mapping of factors that influence child survival, including education, malnutrition, and disease prevention, in order to better understand the specific obstacles faced in different regions.
Researchers estimated that if every district in the low- and middle-income countries studied had met the Sustainable Development Goal (SDG) target of at least as low as 25 child deaths per 1,000 live births, 2.6 million fewer children would have died. If every district within a country rose to the level of the best-performing district in that country, the estimated number of deaths averted rises to 2.7 million.
The vast majority of the 17,554 districts among the 99 nations studied saw improvement in lowering child deaths, but levels of inequality between districts were more variable over the study period. Despite major gains in reducing child deaths over the past 20 years, the highest rates of death in 2017 were still largely concentrated where rates were highest in 2000.
“It is as reprehensible as it is tragic that, on average, nearly 15,000 children under age 5 die every day,” said Dr. Simon I. Hay, the senior author on the study and Director of the Local Burden of Disease (LBD) group at IHME. “Why are some areas doing so well, while others struggle? In order to make progress, we need to enable precise targeting of interventions, such as vaccines. Our findings provide a platform for nations’ health ministers, clinicians, and others to make focused improvements in health systems.”
The study, funded by the Bill & Melinda Gates Foundation, reveals areas of success where strategies could be replicated across and within countries, according to Dr. Hay.
For example, in Rwanda, the highest district-level rate of child deaths in 2017 was less than half that of the lowest district-level death rate in 2000 – gains partially attributed to investments in children’s health in the poorest communities, expansion of health insurance, and increasing numbers of community health workers. Nepal significantly decreased inequalities among its districts over the study period. And Peru made major strides in reducing child mortality and inequality after implementing sustained, cross-cutting antipoverty and health programs.
The study estimates both rates and absolute numbers of deaths by district, presenting a complete picture of global child mortality that illuminates important trends and patterns.
A growing proportion of child deaths are occurring in areas with low overall death rates. Neonatal mortality (death occurring in a child’s first 28 days) and infant mortality (death in the first year of life) are both increasing as a percentage of total child deaths. These trends highlight the need for tailored approaches.
Hay and his research team are working toward more detailed mapping of factors that influence child survival, including education, malnutrition, and disease prevention, in order to better understand the specific obstacles faced in different regions.
| Among the key findings:
|
The LBD project produces estimates of health outcomes and related measures covering entire continents at a fine geographic resolution. Project leaders are seeking additional collaborators, including academics, researchers, and others, to contribute data and evaluate draft papers. For more information, please contact the LBD Engagement Team at [email protected].
All estimates produced from this research are publicly available at the Global Health Data Exchange: http://ghdx.healthdata.org.
In this press release, we use the term “district” to refer to second administrative subdivisions within a country. This does not align perfectly with naming conventions in every country mapped. For information on individual countries, please see the accompanying FAQ or reach out to our media team.
All estimates produced from this research are publicly available at the Global Health Data Exchange: http://ghdx.healthdata.org.
In this press release, we use the term “district” to refer to second administrative subdivisions within a country. This does not align perfectly with naming conventions in every country mapped. For information on individual countries, please see the accompanying FAQ or reach out to our media team.